Image by Gerd Altmann from Pixabay
Writer: Lento Yamagata
Editor: Altay Shaw
What comes to mind when the phrase “gut microbiota” is mentioned? Interest in this component of the body has skyrocketed during recent years, with the search frequency of this term alone going up fivefold this year alone, according to Google. However, with the ever-growing slew of information regarding this topic online, things can rapidly become overwhelming. What exactly is your gut microbiota, and how could it link to treatments for cancer?
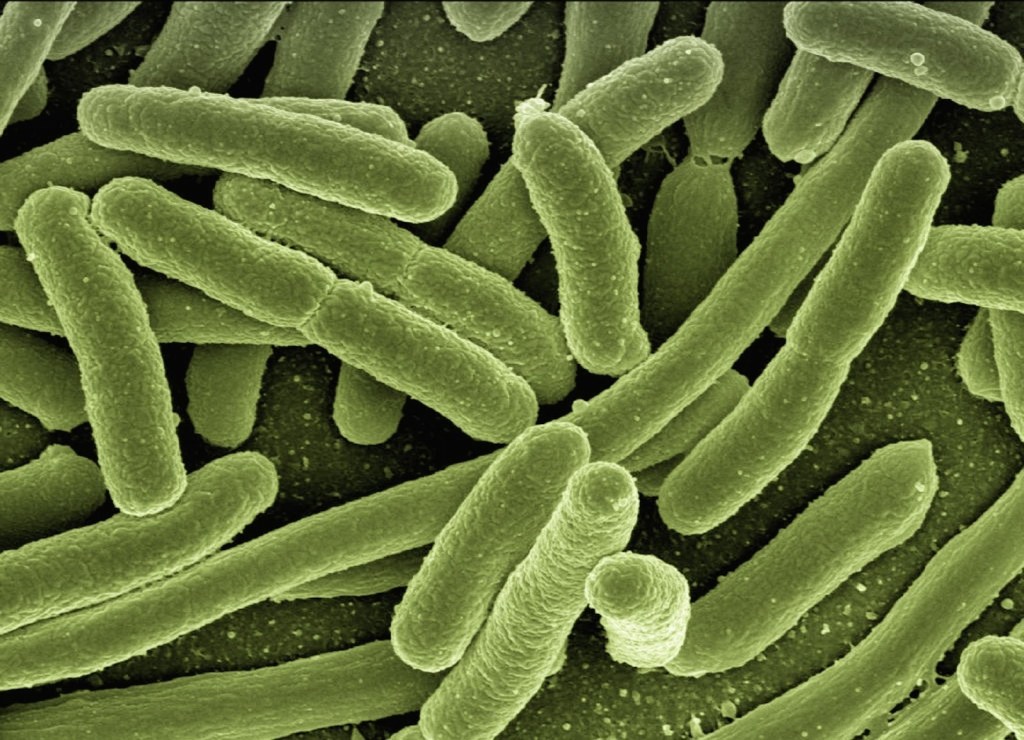
Your gut microbiota refers to the collective population of commensal (helpful) bacteria, fungi, and viruses in your small and large intestines. This is distinct from the similarly named gut microbiome, which also includes the genetic material of the microbiota and environment affecting your gut microbiota. Initially, the first function discovered by the gut microbiota was the digestion and fermentation of foods that could not be easily digested by our cells, including the breakdown of complex fibres and short-chain fatty acid production. Inflammatory bowel diseases like Crohn’s disease can also be associated with the dysregulation of microbiota.
Over time, several other functions outside of digestion have been discovered. Particularly noteworthy among these are the impacts on the immune system and the body’s anti-cancer reactions. Antibiotics have been shown to negatively affect the body’s ability to respond to immunotherapy treatments in multiple different cancers, including renal and non-small cell lung sarcoma (NSCLS). Due to the relatively indiscriminate nature of these antibiotics, scientists focused on a particular strain of interest, Faecalibacterium prasunitzii, associated with decreased inflammation and improved immune response.
Recently, a study in 2024 by Bredon M. et al. expanded on these studies by showing that the specific composition of certain species of bacteria in the gut significantly affects the response of the body to current cancer chemotherapies in both lung cancer and melanoma. First, data analysis of two independent studies on human advanced melanoma and NSCLC was done to show association of elevated F. prasunitzii with a good response to immune checkpoint immunotherapy. This treatment weakens immune system resistance to cancers by blocking the switch that cancer cells commonly express, PD-L1, to turn off cancer-fighting T cells. The study then confirmed F. prasunitzii also being elevated correlated with improved response to PD-L1 in a live mouse cancer model.
However, the phase II clinical trial for F. prasunitzii strain EXL01 did not induce any change in the faecal microbiota composition when administered orally in patients, suggesting the bacteria directly interacts with small intestine immune cells. Already, new research is tackling these specific interactions between gut bacteria and immune cells. One study by Shi et al. 2025 showed a correlation between the butyrate metabolite produced by F. prasunitzii and the increased efficacy of PD-L1 in natural killer/T-cell lymphoma, a promising result for this next-gen probiotic.
So, the next time you read about the gut microbiota, remember that it could be the key to a new way of fighting cancer!
