Author: Mia McDonald Rose
Editor: Altay Shaw
World AIDS Day 2024 marks another year of progress. As we strive to eradicate the epidemic by 2030, the fight is far from over.

For decades, advocates like Jesse Jackson have stood strong for HIV-positive individuals, demanding fair research, better healthcare and an end to the stigma. Source: Getty Images
Spilling into the auditorium, it was inspiring to be amongst a group responsible for changing the lives of so many. An assembly of health workers, researchers and advocates who for years have been on the frontline of the war on AIDS. Now, they are gathered together at the Francis Crick Auditorium to reflect and rejoice over their victories. Friday the 1st of December 2024 marks the 37th World AIDS Day, and here in London, the air is electric with the news of the day. Just last night, the Prime Minister pledged £37 million more to the cause: UNAIDS 2030—a global mission to stop the AIDS epidemic by 2030.
Many of the scheduled speakers have spent decades dedicated to this fight, working towards breakthroughs in treating and preventing HIV. Today, their progress has benefited countless individuals and families living with HIV. Dr Sheena McCormack, a Professor of Clinical Epidemiology at University College London, is a prominent example. Dr. McCormack highlights that globally, infection rates continue to fall. In 2023 there were only 1.3 million new HIV infections, a 39% decrease since 2010 and a 60% decrease since 1995. “I do think we should be positive about that. It’s not as low as we want it, but it is the lowest we have seen yet,” says McCormack.
Though in a sobering contrast, she also highlights that across the world, 9.3 million people who are living with HIV remain untreated. “That’s a crime that we have to do something about now”, says McCormack, “society, at the moment, is moving slightly in the wrong direction, we just have to find a way to achieve equitable access.” Overcoming the AIDS crisis is within reach, but with 2030 on the horizon and one life lost every minute to AIDS-related illnesses, time is running out.
Back to the Beginning
The virus responsible for AIDS, the human immunodeficiency virus (HIV), was identified back in 1981. The virus spreads through sexual contact. Left untreated, the infection worsens as the virus multiplies to replace functional immune cells, weakening the body’s immunological defense. At this stage the condition is known as acquired immunodeficiency syndrome (AIDS) and the affected individual is considered vulnerable to secondary infections. HIV infection is a lifelong affliction because there is currently no cure. Anyone found to be HIV-positive in the 1980s was expected to survive for an average of only one more year. But for those diagnosed today, the outlook is substantially better.
15 years after the emergence of HIV, Anti-retroviral therapy (ART) became available. ART suppresses HIV, preventing it from multiplying. ART is able to protect immunological function and revert the life-span of individuals receiving this treatment back to near normal. But new infections continue to arise, and various barriers such as limited access to treatment have delayed the ending of the AIDS epidemic.
The UNAIDS 2030 elimination goals strive for 95% of people to know if they have HIV, 95% of those with HIV to be on ART treatment and 95% virally suppressed. The main obstacle in achieving these targets is health inequity—disparities in health outcomes that stem from systemic inequalities. Expensive treatments and harmful stigmas are an enduring hindrance to HIV-positive individuals, leaving many without access to critical care. Unlike with other deadly viruses, no successful vaccine has been developed for HIV. Four decades into the crisis, the United Nations is spearheading the 2030 mission with the hope of stopping the spread of HIV, for good.
Tackling HIV in England
In England, the National Aids Trust (NAT) has been a key player in bringing the 2030 objective to the government’s attention. In 2021, the NAT established a commission of HIV experts who mapped out an action plan for England to accomplish by 2025. The plan aimed to cut new HIV diagnoses by 80% and achieve a 50% decline in AIDS-related deaths. But now, 2025 is upon us and the targets have not been met. James Cole of the National Aids Trust points out that “unfortunately, we are off track.”
Now, the Trust has put forward a new action plan dubbed ‘Getting on track: Becoming the first country to end New HIV Cases by 2030′. The new report outlines six key goals and policy recommendations, including improving treatment and prevention access. Another key recommendation is expanding access to HIV screening, Cole stresses that “we must find everyone living with undiagnosed HIV in England.”
Statistics estimate that over 113,000 people live with HIV in the UK, but that a significant proportion remain undiagnosed. If England is to be the first country to end new HIV cases, it is vital the new NAT action plan outlined is valued and addressed because in the UK, HIV transmission rates are not falling, but rising.
Diagnostic Trends
In 2023, new HIV diagnoses rose by 15% in the UK, reflecting broader trends among heterosexual men and women that have been steadily rising since 2020. While in the past, HIV has disproportionately affected men who have sex with men, since 2014, there has been a 44% decline in new HIV diagnoses in this group. However, upon accounting for ethnicity, these gains only reflect white men, with no decline seen within minority populations.
While case numbers continue to climb, many of these new HIV diagnoses come too late, when the virus has already progressed to AIDS. Late diagnoses are recognized as a public health concern as a heavy burden on the afflicted individual as well as the national health service. So accordingly, of the funds committed by the Prime Minister on World Aids Day this year, £27 million will be used to expand wider access to HIV screening.
In sexual health centers, availability of testing has recently improved, but overall HIV screening levels still remain lower than before the COVID-19 pandemic. Against the backdrop of funding cuts, rural communities are particularly underserved by sexual health services, but are facing an ever-growing demand.
The new government funding hopes to address this urgent need for better testing by supporting the roll-out of HIV screening in emergency departments across the country. The new opt-out test will offer an HIV test to anyone providing a blood sample. “It was really welcome to see strong commitments from the Prime Minister” says Cole.

New cases of HIV infection have been steadily lowering since the virus’s peak in 1995, but with 1.3 million new infections in 2023, the fight is not yet finished. Made in Canva.
The Prevention Evolution: PrEP
While facilitating widespread screening is of vital importance, improving access to HIV preventatives will be equally impactful in the race to end HIV in England.
One of the speakers today, Dr Sheena McCormack, was part of a 2015 clinical team that studied preventative drugs in a real-world setting. The ‘PROUD’ trial revealed that the drugs used had successfully lowered the risk of HIV infections by 86%. The results of the study influenced the World Health Organization updated their guidelines to recommend the preventatives to anyone at a high risk of HIV exposure. Now dubbed as a Pre-Exposure Prophylaxis (PrEP), the oral medication was commissioned by the NHS In 2020 and around 90,000 people are taking PrEP in the UK today.
Discussing the impacts, McCormack reflects that “It was a kind of joyous time, because as a researcher, if you do a study and you get a result, you do want to see it make a public health impact.” However, McCormack also notes that PrEP uptake has not been consistent across all demographics, with studies failing to show a reduced HIV transmission risk for women. “We’ve got a really clear explanation for what it is, and it seems to be adherence. It’s not that the drugs don’t work,” says McCormack.
While certain high-risk groups are easier to identify, women at risk of HIV are proving hard to treat. Winnie Ssanyu Sseruma, an influential AIDS activist also touches on this issue, “PrEP is good for gay men and bisexual men, and I think women don’t feel included, there’s this lack of information, you know, a resistance that maybe this is not for us.” Translating the successes of PrEP to all high-risk groups will be a crucial step in meeting the prevention targets for the NAT’s action plan.
Lenacapavir as the New Standard of Prevention?
Though, even as health services work to improve access to PrEP, a promising new drug is already on the horizon. Lenacapavir is a drug originally developed as an antiretroviral treatment for HIV-positive individuals, but it offered little hope in improving outcomes. In the case of prevention however, a clinical trial performed by pharmaceutical company Gilead dubbed PURPOSE, demonstrated that Lenacapavir can successfully stop new HIV infections.
The PURPOSE study tested Lenacapavir as a twice-yearly injection, assessing three cohorts of cisgender women. One cohort were administered Lenacapavir while the other two groups received once-daily oral medication for prevention. Among the Lenacapavir group, there were 0 cases of HIV infection.After injected, Lenacapavir is effective for six months and is therefore the closest any medication has come to an HIV vaccine. Lenacapavir was awarded Science’s 2024 Breakthrough of the Year.
Discussing the new preventative, McCormack says that “It was the second occasion when I’ve been at an AIDS conference, where the audience stood up and applauded the presenter.” Similarly to the impact of the PROUD trial, the results of the Gilead studies influenced the WHO to revise their guidelines to recommend Lenacapavir as another form of PrEP.
As a long-lasting preventative, Lenacapavir is well-suited to guarantee medication compliance, particularly in rural communities where resources are limited. But as is the case with other preventatives, securing broader access has been a struggle. The Gilead trial took place in Sub-Saharan Africa, where over half of the global population living with HIV resides. But despite the insights this region provided to the studies, access to the medication here is limited. Charities such as STOPAIDS are calling for their governments to influence pharmaceutical companies to ensure that the promising new medication will be affordable to all who need it.

Lenacapavir was awarded Science’s 2024 Breakthrough of the Year and has revolutionised HIV prevention strategies. Source: Alamy
Persisting Stigma
In the race to end the AIDS epidemic by 2030, inadequate access to treatment continues to impede global progress. But overcoming harmful stigma remains another challenge. Negative perceptions surrounding HIV are pervasive in England. Last year, one in seven people living with HIV avoided healthcare because they feared stigma. Even in England, a country thought to more socially advanced, stigma is a factor reinforcing health inequities felt by HIV-positive individuals. “This really is unacceptable today and is pushing us further back within the response” says James Cole of the NAT, “people must feel confident in accessing healthcare services free from stigma and discrimination.”
Misinformation has surrounded the AIDS crisis from the very beginning and discrimination against those living with HIV persists, in part due to the belief that HIV-positive individuals are highly infectious. Dr Andrew Phillips, an epidemiologist at UCL worked on a trial in 2014 that helped to disprove such ignorant perceptions. The PARTNER trial demonstrated that individuals living with HIV who are taking antiretroviral treatment to the extent of viral suppression are not infectious to even their sexual partners.
The trial was pivotal in disproving harmful HIV stigmas and sparked the U=U statement that stands for undetectable=untransmissible. “People say that that improves certainly their own self-esteem, but also other people’s perceptions. So hopefully we’re getting there slowly as people become more educated about it, but it’s still a huge challenge” says Phillips. With the aim to break down HIV stigma further, the other £10 million of the funds committed by the government on World Aids Day will go toward the Robert Carr Fund. With the purpose to defend the rights of those marginalized by HIV and AIDS stigma, not just in the UK, but across the globe.
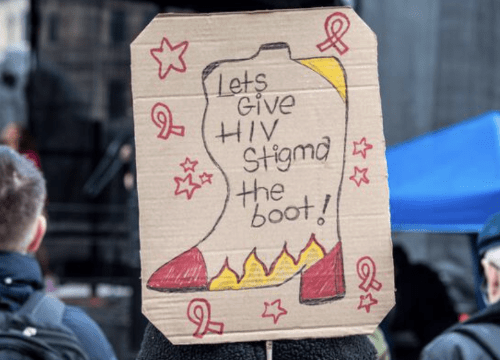
HIV stigma is a major barrier to ending the epidemic. Thanks to the hard work of activists, public attitudes towards those living with HIV have improved. Source: Alamy
The Power of Advocacy
The final speaker of the day, Winnie Ssanyu Sseruma, shares her own experience as an advocate for those living with HIV. Winnie brings a new perspective to the stage, as someone who has been diagnosed with HIV. “The challenges overshadow what is going on the ground. Many people’s lives have been transformed and continue to do so,” says Winnie.
Each speaker today has mapped out breakthroughs in HIV screening, prevention and treatment that together, have brought us to the brink of ending the epidemic. It has been a painful journey. When the virus emerged, death and despair were the harsh reality among those diagnosed, but today, the lives of those affected by HIV can be radically different. As we reflect on this transformation today, a distinct sense of pride can be felt radiating through the conference center. The dedication of the individuals in this room alludes to a powerful community, not seen within other research fields.
Engaged in the war on AIDS from the beginning, many individuals here have advocated and defended the rights of people living with HIV. “HIV advocates are different, because we get into the science. Instead of throwing buckets of red paint at pharmaceutical companies, we sit around the table and talk to them” says Winnie. Via this approach, a great deal has been achieved. Ethical research and accessible treatment have been secured for millions, despite the ongoing setbacks caused by societal stigma.
Now, the end is within reach and If England and beyond is to succeed in stopping the spread of HIV by 2030, eliminating barriers must take precedence. The fight to overcome stigma and eradicate health inequity continues, with many individuals still untreated and unsupported. But Winnies’ final words drive home the lasting impact of the cause. “We live with the condition. We take the pills. We are the people who are being talked about when they say treatment is working. We were fighting for our lives and this saved our lives.”
